Search for drugs:
Typing the drug name to query
ZIPRASIDONE HYDROCHLORIDE
DIR Classification
Classification:Most-DIR concern
Severity Score:4
Description in Drug Labeling: View Full Labeling: SPL in DailyMed | PDF
- WARNINGS AND PRECAUTIONS
- QT Prolongation and Risk of Sudden Death
- Ziprasidone use should be avoided in combination with other drugs that are known to prolong the QTc interval [see CONTRAINDICATIONS (4.1) and DRUG INTERACTIONS (7.4)]. Additionally, clinicians should be alert to the identification of other drugs that have been consistently observed to prolong the QTc interval. Such drugs should not be prescribed with ziprasidone. Ziprasidone should also be avoided in patients with congenital long QT syndrome and in patients with a history of cardiac arrhythmias [see CONTRAINDICATIONS (4)].
- A study directly comparing the QT/QTc prolonging effect of oral ziprasidone with several other drugs effective in the treatment of schizophrenia was conducted in patient volunteers. In the first phase of the trial, ECGs were obtained at the time of maximum plasma concentration when the drug was administered alone. In the second phase of the trial, ECGs were obtained at the time of maximum plasma concentration while the drug was co-administered with an inhibitor of the CYP4503A4 metabolism of the drug.
- In the first phase of the study, the mean change in QTc from baseline was calculated for each drug, using a sample-based correction that removes the effect of heart rate on the QT interval. The mean increase in QTc from baseline for ziprasidone ranged from approximately 9 to 14 msec greater than for four of the comparator drugs (risperidone, olanzapine, quetiapine, and haloperidol), but was approximately 14 msec less than the prolongation observed for thioridazine.
- In the second phase of the study, the effect of ziprasidone on QTc length was not augmented by the presence of a metabolic inhibitor (ketoconazole 200 mg twice daily).
- In placebo-controlled trials, oral ziprasidone increased the QTc interval compared to placebo by approximately 10 msec at the highest recommended daily dose of 160 mg. In clinical trials with oral ziprasidone, the electrocardiograms of 2/2988 (0.06%) patients who received ziprasidone hydrochloride and 1/440 (0.23%) patients who received placebo revealed QTc intervals exceeding the potentially clinically relevant threshold of 500 msec. In the ziprasidone-treated patients, neither case suggested a role of ziprasidone. One patient had a history of prolonged QTc and a screening measurement of 489 msec; QTc was 503 msec during ziprasidone treatment. The other patient had a QTc of 391 msec at the end of treatment with ziprasidone and upon switching to thioridazine experienced QTc measurements of 518 and 593 msec.
- Some drugs that prolong the QT/QTc interval have been associated with the occurrence of torsade de pointes and with sudden unexplained death. The relationship of QT prolongation to torsade de pointes is clearest for larger increases (20 msec and greater) but it is possible that smaller QT/QTc prolongations may also increase risk, or increase it in susceptible individuals. Although torsade de pointes has not been observed in association with the use of ziprasidone in premarketing studies and experience is too limited to rule out an increased risk, there have been rare post-marketing reports (in the presence of multiple confounding factors) [see ADVERSE REACTIONS (6.2)].
- As with other antipsychotic drugs and placebo, sudden unexplained deaths have been reported in patients taking ziprasidone at recommended doses. The premarketing experience for ziprasidone did not reveal an excess risk of mortality for ziprasidone compared to other antipsychotic drugs or placebo, but the extent of exposure was limited, especially for the drugs used as active controls and placebo. Nevertheless, ziprasidone’s larger prolongation of QTc length compared to several other antipsychotic drugs raises the possibility that the risk of sudden death may be greater for ziprasidone than for other available drugs for treating schizophrenia. This possibility needs to be considered in deciding among alternative drug products [see INDICATIONS AND USAGE (1)].
- Certain circumstances may increase the risk of the occurrence of torsade de pointes and/or sudden death in association with the use of drugs that prolong the QTc interval, including (1) bradycardia; (2) hypokalemia or hypomagnesemia; (3) concomitant use of other drugs that prolong the QTc interval; and (4) presence of congenital prolongation of the QT interval.
- It is recommended that patients being considered for ziprasidone treatment who are at risk for significant electrolyte disturbances, hypokalemia in particular, have baseline serum potassium and magnesium measurements. Hypokalemia (and/or hypomagnesemia) may increase the risk of QT prolongation and arrhythmia. Hypokalemia may result from diuretic therapy, diarrhea, and other causes. Patients with low serum potassium and/or magnesium should be repleted with those electrolytes before proceeding with treatment. It is essential to periodically monitor serum electrolytes in patients for whom diuretic therapy is introduced during ziprasidone treatment. Persistently prolonged QTc intervals may also increase the risk of further prolongation and arrhythmia, but it is not clear that routine screening ECG measures are effective in detecting such patients. Rather, ziprasidone should be avoided in patients with histories of significant cardiovascular illness, e.g., QT prolongation, recent acute myocardial infarction, uncompensated heart failure, or cardiac arrhythmia. Ziprasidone should be discontinued in patients who are found to have persistent QTc measurements >500 msec.
- For patients taking ziprasidone who experience symptoms that could indicate the occurrence of torsade de pointes, e.g., dizziness, palpitations, or syncope, the prescriber should initiate further evaluation, e.g., Holter monitoring may be useful.
- [Patients with Concomitant Illness]
- Ziprasidone has not been evaluated or used to any appreciable extent in patients with a recent history of myocardial infarction or unstable heart disease. Patients with these diagnoses were excluded from premarketing clinical studies. Because of the risk of QTc prolongation and orthostatic hypotension with ziprasidone, caution should be observed in cardiac patients. [see WARNINGS AND PRECAUTIONS (5.3), (5.9)].
- DRUG INTERACTIONS
- Pharmacodynamic Interactions
- Ziprasidone should not be used with any drug that prolongs the QT interval [see CONTRAINDICATIONS (4.1)].
- CONTRAINDICATIONS
- QT Prolongation
- Because of ziprasidone’s dose-related prolongation of the QT interval and the known association of fatal arrhythmias with QT prolongation by some other drugs, ziprasidone is contraindicated:
- in patients with a known history of QT prolongation (including congenital long QT syndrome)
- in patients with recent acute myocardial infarction
- in patients with uncompensated heart failure
- Pharmacokinetic/pharmacodynamic studies between ziprasidone and other drugs that prolong the QT interval have not been performed. An additive effect of ziprasidone and other drugs that prolong the QT interval cannot be excluded. Therefore, ziprasidone should not be given with:
- dofetilide, sotalol, quinidine, other Class Ia and III anti-arrhythmics, mesoridazine, thioridazine, chlorpromazine, droperidol, pimozide, sparfloxacin, gatifloxacin, moxifloxacin, halofantrine, mefloquine, pentamidine, arsenic trioxide, levomethadyl acetate, dolasetron mesylate, probucol or tacrolimus.
- other drugs that have demonstrated QT prolongation as one of their pharmacodynamic effects and have this effect described in the full prescribing information as a contraindication or a boxed or bolded warning [see WARNINGS AND PRECAUTIONS (5.3)].
- OVERDOSAGE
- Management of Overdosage
- Cardiovascular monitoring should commence immediately and should include continuous electrocardiographic monitoring to detect possible arrhythmias. If antiarrhythmic therapy is administered, disopyramide, procainamide, and quinidine carry a theoretical hazard of additive QT-prolonging effects that might be additive to those of ziprasidone.
- ADVERSE REACTIONS
- Clinical Trials Experience
- ECG Changes - Ziprasidone is associated with an increase in the QTc interval [see WARNINGS AND PRECAUTIONS (5.3)]. In the schizophrenia trials, ziprasidone was associated with a mean increase in heart rate of 1.4 beats per minute compared to a 0.2 beats per minute decrease among placebo patients.
- PATIENT COUNSELING INFORMATION
- QTc Prolongation
- Advise patients to inform their health care providers of the following: History of QT prolongation; recent acute myocardial infarction; uncompensated heart failure; prescription of other drugs that have demonstrated QT prolongation; risk for significant electrolyte abnormalities; and history of cardiac arrhythmia [see CONTRAINDICATIONS (4.1) and WARNINGS AND PRECAUTIONS (5.3)].
- Instruct patients to report the onset of any conditions that put them at risk for significant electrolyte disturbances, hypokalemia in particular, including but not limited to the initiation of diuretic therapy or prolonged diarrhea. In addition, instruct patients to report symptoms such as dizziness, palpitations, or syncope to the prescriber [see WARNINGS AND PRECAUTIONS (5.3)].
- INDICATIONS AND USAGE
- Ziprasidone capsules are indicated for the treatment of schizophrenia, as monotherapy for the acute treatment of bipolar manic or mixed episodes, and as an adjunct to lithium or valproate for the maintenance treatment of bipolar disorder. When deciding among the alternative treatments available for the condition needing treatment, the prescriber should consider the finding of ziprasidone’s greater capacity to prolong the QT/QTc interval compared to several other antipsychotic drugs [see WARNINGS AND PRECAUTIONS (5.3)]. Prolongation of the QTc interval is associated in some other drugs with the ability to cause torsade de pointes-type arrhythmia, a potentially fatal polymorphic ventricular tachycardia, and sudden death. In many cases this would lead to the conclusion that other drugs should be tried first. Whether ziprasidone will cause torsade de pointes or increase the rate of sudden death is not yet known [see WARNINGS AND PRECAUTIONS (5.3)]
Postmarketing Surveillance
Contingency Table:
Current Drug
Other Drugs
Rhabdomyolysis
94
42818
Other ADRs
12823
14104456
Odds Ratio = 2.415
Drug Property Information
ATC Code(s):
- N05AE04 - ziprasidone hydrochloride
- N05AE - Indole derivatives
- N05A - ANTIPSYCHOTICS
- N05 - PSYCHOLEPTICS
- N - NERVOUS SYSTEM
Active Ingredient:ziprasidone hydrochloride
Active Ingredient UNII:216X081ORU
Drugbank ID:DB00246
PubChem Compound:60854
CAS Number:146939-27-7
Dosage Form(s):capsule
Route(s) Of Administrator:oral
Daily Dose:
- 80.0 mg/day N05AE04
Chemical Structure: 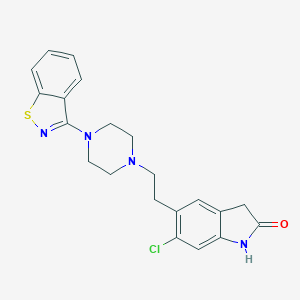
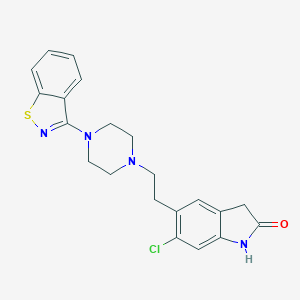
SMILE Code:
C1CN(CCN1CCC2=C(C=C3C(=C2)CC(=O)N3)Cl)C4=NSC5=CC=CC=C54
C1CN(CCN1CCC2=C(C=C3C(=C2)CC(=O)N3)Cl)C4=NSC5=CC=CC=C54
Reference
COHORT STUDY:
N/AOTHER REFERENCE(S):
N/ADisclaimer:
The content of this database of rhabdomyolysis is intended for educational and scientific research purposes only. It is not intended as a substitute for professional medical advice, diagnosis or treatment.
The views presented in this website do not necessarily reflect current or future opinion or policy of the US Food and Drug Administration. Any mention of commercial products is for clarification and not intended as endorsement.